 Undergoing a surgery is always a nerve-wracking experience. You want to be able to trust that your surgeon conducted and reviewed the appropriate pre-operative tests. Can a surgeon be held liable if he or she fails to review the results of the pre-operative tests before performing the surgery?
Undergoing a surgery is always a nerve-wracking experience. You want to be able to trust that your surgeon conducted and reviewed the appropriate pre-operative tests. Can a surgeon be held liable if he or she fails to review the results of the pre-operative tests before performing the surgery?
Roger Burchfield was admitted to Willis-Knighton Medical Center to receive non-emergency surgery on his gallbladder. Before the surgery, Burchfield’s surgeon, Forrest Wright, ordered a chest x-ray and EKG. However, Wright did not review the results prior to performing the surgery. If Wright had reviewed the tests, he would have seen Burchfield had congestive heart failure and multiple other possible heart issues. Burchfield himself did not know he had these heart issues.
The surgery was successful, and Burchfield went home. However, about a day later, Burchfield started experiencing swelling. He went to the emergency room and was admitted into the hospital. The hospital found Burchfield had suffered a heart infection, respiratory failure, heart failure, and other issues. He was put in a medically induced coma before undergoing a heart transplant. Although Burchfield recovered from the transplant, he was no longer able to work as a mechanic and requires medical care for the transplant for the rest of his life.
 Louisiana Personal Injury Lawyer Blog
Louisiana Personal Injury Lawyer Blog


 If the trial court does not rule in your favor, you might find yourself considering filing an appeal. However, just like filing an initial lawsuit, there are strict time limits for filing an appeal. If you do not comply with these time limits, the appellate court will be unable to consider the merits of your appeal, and you will be stuck with the trial court’s ruling.
If the trial court does not rule in your favor, you might find yourself considering filing an appeal. However, just like filing an initial lawsuit, there are strict time limits for filing an appeal. If you do not comply with these time limits, the appellate court will be unable to consider the merits of your appeal, and you will be stuck with the trial court’s ruling.  In the face of the profound loss that accompanies the passing of a family member, the impact can be particularly agonizing when that loss follows the anticipation of medical intervention, such as a transplant. The immediate inclination might be to explore legal avenues through a medical malpractice claim, yet the determination of whether negligence played a role can be an intricate matter for the average individual. This Louisiana case shows how important it can be to obtain expert testimony to help show malpractice occurred.
In the face of the profound loss that accompanies the passing of a family member, the impact can be particularly agonizing when that loss follows the anticipation of medical intervention, such as a transplant. The immediate inclination might be to explore legal avenues through a medical malpractice claim, yet the determination of whether negligence played a role can be an intricate matter for the average individual. This Louisiana case shows how important it can be to obtain expert testimony to help show malpractice occurred. 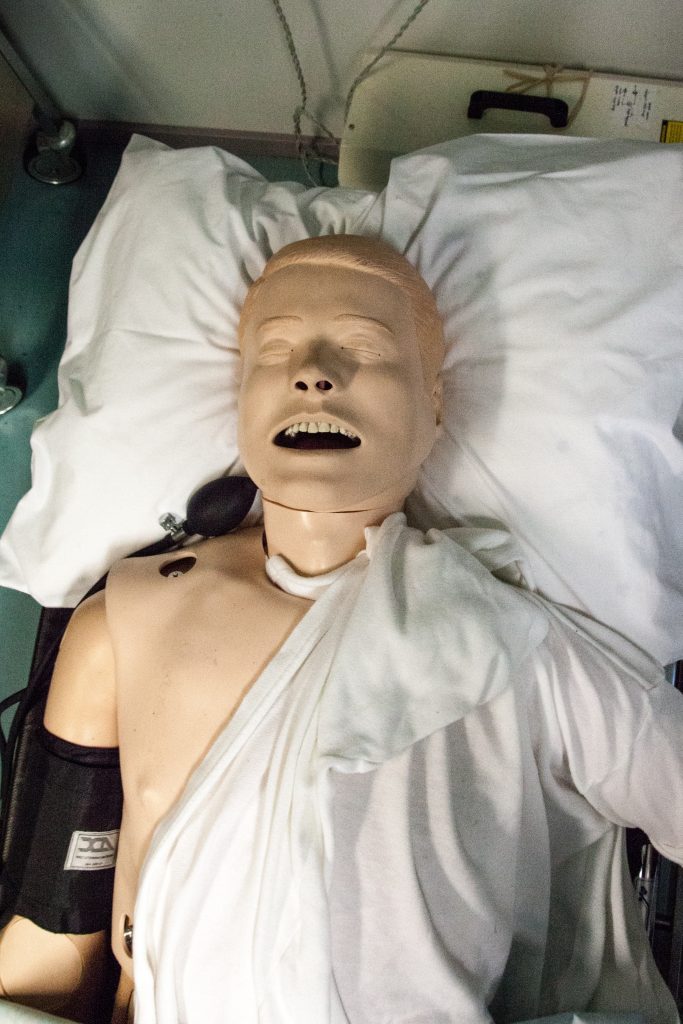 The prospect of undergoing medical procedures carries inherent risks; sometimes, unfortunate incidents can lead to injuries. In such cases, individuals can pursue medical malpractice claims to seek compensation for damages. A crucial aspect of these claims is presenting the appropriate evidence and adhering to procedural requirements. A telling illustration of the importance of these procedures is found in a lawsuit involving Elliott R. James and Lakeview Medical Center, LLC. This case underscores the significance of following legal protocols and obtaining substantial evidence to bolster a medical malpractice claim.
The prospect of undergoing medical procedures carries inherent risks; sometimes, unfortunate incidents can lead to injuries. In such cases, individuals can pursue medical malpractice claims to seek compensation for damages. A crucial aspect of these claims is presenting the appropriate evidence and adhering to procedural requirements. A telling illustration of the importance of these procedures is found in a lawsuit involving Elliott R. James and Lakeview Medical Center, LLC. This case underscores the significance of following legal protocols and obtaining substantial evidence to bolster a medical malpractice claim. When medical emergencies strike, the rapid response of emergency medical technicians (EMTs) can mean the difference between life and death. However, the high-pressure nature of their role can also give rise to complex legal questions when outcomes take a tragic turn. Richard Miller’s case sheds light on the intricate landscape of EMT liability, illuminating the balance between legal protections afforded to these healthcare professionals and the pursuit of justice for patients and their families. It also helps answer the question: Can an emergency medical technician or their employer be held liable when things go wrong?
When medical emergencies strike, the rapid response of emergency medical technicians (EMTs) can mean the difference between life and death. However, the high-pressure nature of their role can also give rise to complex legal questions when outcomes take a tragic turn. Richard Miller’s case sheds light on the intricate landscape of EMT liability, illuminating the balance between legal protections afforded to these healthcare professionals and the pursuit of justice for patients and their families. It also helps answer the question: Can an emergency medical technician or their employer be held liable when things go wrong?  In the realm of medical malpractice, the intricacies of the legal process can often appear daunting, especially when juxtaposed against the heart-wrenching backdrop of a stillborn baby’s tragedy. K Arceneaux found herself entangled in this very confluence of circumstances, seeking justice for her devastating loss while grappling with legal procedure demands. As the mother’s quest for accountability unfolds, a crucial question emerges: Can a plaintiff prevail in a medical malpractice case without the indispensable backing of expert testimony?
In the realm of medical malpractice, the intricacies of the legal process can often appear daunting, especially when juxtaposed against the heart-wrenching backdrop of a stillborn baby’s tragedy. K Arceneaux found herself entangled in this very confluence of circumstances, seeking justice for her devastating loss while grappling with legal procedure demands. As the mother’s quest for accountability unfolds, a crucial question emerges: Can a plaintiff prevail in a medical malpractice case without the indispensable backing of expert testimony? Many of us provide support to elderly folks in our lives through our time and money. We expect the utmost attention and respect when we send a loved one to a care facility. Sometimes accidents happen, whether by negligence or by accident, that result in injury to patients. Regardless of the cause of injury, a lawsuit can help hold medical professionals responsible for the type of care they provide. The difference between a tort and a medical malpractice claim for nursing home injuries is examined in the following case.
Many of us provide support to elderly folks in our lives through our time and money. We expect the utmost attention and respect when we send a loved one to a care facility. Sometimes accidents happen, whether by negligence or by accident, that result in injury to patients. Regardless of the cause of injury, a lawsuit can help hold medical professionals responsible for the type of care they provide. The difference between a tort and a medical malpractice claim for nursing home injuries is examined in the following case.  When it comes to medical malpractice, time can be both a friend and a foe. Trusting doctors to safeguard the well-being of our loved ones makes the process of bringing a lawsuit challenging and emotionally charged. Yet, within the legal field, there exist specific time frames and procedural intricacies that can make or break a case. Once the clock runs out on a particular timeframe, a lawsuit is deemed barred, leaving individuals without recourse. In the midst of this intricate dance between justice and time, the story of Rita Foster and her family shines a light on the importance of understanding legal procedures and seeking qualified legal representation.
When it comes to medical malpractice, time can be both a friend and a foe. Trusting doctors to safeguard the well-being of our loved ones makes the process of bringing a lawsuit challenging and emotionally charged. Yet, within the legal field, there exist specific time frames and procedural intricacies that can make or break a case. Once the clock runs out on a particular timeframe, a lawsuit is deemed barred, leaving individuals without recourse. In the midst of this intricate dance between justice and time, the story of Rita Foster and her family shines a light on the importance of understanding legal procedures and seeking qualified legal representation. Amid the potential chaos and life-or-death scenarios in a hospital emergency room, “negligent credentialing” might not immediately come to mind. It’s understandable; after all, numerous nightmare scenarios occupy our thoughts. However, negligent credentialing is an incredibly significant matter that hospitals face regularly.
Amid the potential chaos and life-or-death scenarios in a hospital emergency room, “negligent credentialing” might not immediately come to mind. It’s understandable; after all, numerous nightmare scenarios occupy our thoughts. However, negligent credentialing is an incredibly significant matter that hospitals face regularly. Medical malpractice claims typically involve allegations of negligence during a medical procedure. However, the following case presents a unique scenario where the alleged injury occurred after the procedure was completed. It examines the legal considerations and challenges in such situations, emphasizing the importance of evidence and expert testimony in establishing a breach of the applicable standard of care.
Medical malpractice claims typically involve allegations of negligence during a medical procedure. However, the following case presents a unique scenario where the alleged injury occurred after the procedure was completed. It examines the legal considerations and challenges in such situations, emphasizing the importance of evidence and expert testimony in establishing a breach of the applicable standard of care.